An Investigational Study on the Use of a Sporicidal Disinfectant to Decontaminate Hazardous Drug Residues on IV Bags
Mark Wiencek, PhD | Contec, Inc.
Michael Bedenbaugh, PharmD, MBA, MS | Intramed Plus, Inc.
Lauren Pernot, BS | Contec, Inc.
Kate Douglass, MS, RN | Cognitive Design Associates
INTRODUCTION
Containers for compounded sterile preparations (e.g., IV bags, syringes, elastomeric pumps) are subject to intense quality control by manufacturers, including sterility validations for the absence of foreign matter or substances. However, once they are received into health care organizations, the responsibility to maintain their integrity and hygiene during compounding and administration shifts to pharmacy and nursing personnel.
PeridoxRTU® Sporicidal Disinfectant Cleaner (PAA/HP) is a sporicidal, fungicidal, and bactericidal 1-step disinfectant registered with the Environmental Protection Agency. The product is commonly used to disinfect surfaces in compounding pharmacies and clean rooms. Additionally, some facilities that compound hazardous drugs (HDs) use a wiping or mopping protocol with chemical agents such as PAA/HP to decontaminate surfaces that may harbor HD residues. Results of previous studies using PAA/ HP with wipes or mop pads on surfaces such as stainless steel, plastic, and vinyl have demonstrated reductions exceeding 99.99% of several marker HDs.1 However, decontamination of residual HDs by wiping final compounded sterile preparation (CSP) containers with PAA/HP has not been studied previously.
IV bags often are composed of multiple layers of polymers, including polyvinyl chloride (PVC), ethylene vinyl acetate (EVA), polypropylene (PP), polyethylene, or a combination of these polymers. The goal for design and construction of bags is to maximize puncture resistance and maintain sterility while ensuring the materials are safe to contact the IV fluids for a prolonged duration.2 Design features also include the use of materials that can be sterilized while minimizing the cost and complexity of manufacturing. The bags may be supplied empty or prefilled with different IV fluids. Most, but not all, IV bags also are sealed inside an outer bag called an overwrap. The overwrap reduces fluid loss from the IV bag due to osmosis, and further protects the bag and its contents from physical damage or contamination during shipping.
Many facility standard operating procedures (SOPs) require that all supplies be wiped to decrease microbial bioburden before entering the buffer room or crossing the segregated compounding area (SCA) perimeter line. Additionally, compounding pharmacies also wipe final hazardous drug CSP doses after compounding HDs to remove potentially hazardous drug residue. This wiping step can reduce the risk of spreading HD residue outside the negative compounding spaces during transport and exposure during administration. Although HD residue on the outside of IV bags and other containers has been examined in several previous studies, the risk level is unclear.3-10 Regardless, IV bags used for HDs are handled in several steps through compounding, transportation, and administration. Strategies for breaking the chain of transmission of these drug residues to reduce occupational exposure can use many of the same methods employed for decreasing transmission of microbial contamination in health care settings. Thus, it is desirable to explore if a simple protocol such as wiping the bag with a readily available chemical agent can effectively decontaminate HD residues without posing a risk to the fluids inside the bag.
METHODS
TABLE 1 | Container Material of IV Bags in ASTM F-739 Test Protocol to Determine Penetration Resistance
|
Container material
|
Brand (manufacturer)
|
Diluent
|
Container volume
|
Catalog reference
|
|---|---|---|---|---|
|
Polyvinyl chloride
|
Viaflex® (Baxter)¹²
|
NSª
|
1,000 mL
|
2B1324X
|
|
Propylene ethylene copolymer
|
Excel™ (B. Braun)¹³
|
NSª
|
1,000 mL
|
L8000
|
|
Polypropylene
|
E³™(B. Braun)¹⁴
|
NSª
|
1,000 mL
|
E8000
|
|
Ethylene vinyl acetate
|
Pinnacle™ CP0500(B. Braun)¹⁵
|
None
|
500mL
|
2112347
|
aNS: Sodium chloride 0.9% solution
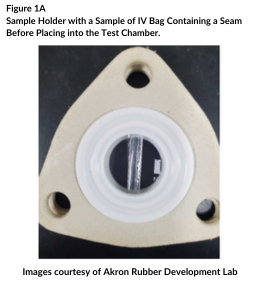
The studies were conducted at the Akron Rubber Development Lab, a laboratory that specializes in testing the penetration resistance of PPE. IV bags were removed from the overwrap, if present, and emptied of fluid. An initial study measured penetration resistance of 3 randomly selected areas (5 cm2) of the 4 types of IV bags, some of which may have included the seams. A second study consisted of single samples (5 cm2) that focused on the seams of each bag (Figure 1A). In each case, the outer face of the IV bag was positioned within the exposure test chamber (Figure 1B) to contact the solution of PAA/HP.
.png?width=260&height=282&name=Images%20courtesy%20of%20Akron%20Rubber%20Development%20Lab%20(1).png)
Over 8 hours, a fresh solution of PAA/HP was recirculated across the surface of the IV bags through a closed-loop system. A blank solution of distilled water was recirculated on the other side of the IV bag sample. It was measured continuously with UV-Vis absorption spectrometry to detect penetration of the PAA/HP solution through the sample. The minimum detection level was 5 parts-per-million (ppm) of PAA/HP solution.
The penetration resistance of IV bags after immersion in a solution of PAA/HP also was determined with a different procedure. This colorimetric assay uses spectrophotometry to measure trace levels of hydrogen peroxide after reaction with a mixture of ferric iron with xylenol orange (PeroxiDetect™ Kit, Sigma-Aldrich). In Europe, several studies have utilized this sensitive assay for peroxides to assess if vapor-phase peracetic acid or hydrogen peroxide can penetrate IV bags during disinfection of isolators and devices used to reconstitute HDs.16-17 This test included samples of IV bags like those listed in Table 1. The Baxter Viaflex® bags used in this study were smaller (250 mL; REF 2B1322) than the bags used in the penetration studies using ASTM Method F-739. The Pinnacle™ EVA bags were prefilled with 500 mL sterile water before the test. The exposure method involved immersing triplicate bags in a solution of PAA/HP up to, but not covering, the septa. After immersing the bags for 1 hour at room temperature, the IV solutions inside the bags were assessed for levels of hydrogen peroxide using the test kit.
An additional study was performed to determine the decontamination of HD residues from the outside of IV bags using wipers wetted with the PAA/HP solution. The outer surface, 7.6 cm x 10.2 cm (3 inches x 4 inches area) of 2 sets of triplicate PVC bags were intentionally contaminated with dilutions of 3 different HDs using a 1 mL syringe/needle as described in Table 2.
Drug solutions were allowed to dry on the outside surface of the bag for 30 minutes inside the containment primary engineering control (CPEC). One set of triplicate samples was used as controls to determine recovery efficiency of the sampling process. The other set of triplicate samples was used to measure the efficacy of decontamination. The decontamination procedure involved wiping each contaminated bag using a single pass with a sterile quarter-folded 9 inch x 9 inch polyester-cellulose wipe saturated with PAA/HP. After 3 minutes, each bag was wiped with a sterile quarter-folded 9 inch x 11 inch polypropylene wipe pre-saturated with sterile 70% isopropyl alcohol/30% water (sIPA). After drying, the area of contamination on each of the 6 bags was sampled using the swabbing technique prescribed in a commercial HD sampling kit.18
TABLE 2 | Hazardous Drug Dilution for Surface Application and Decontamination Testing of IV Bags
|
Drug
|
Diluent
|
Concentration/ reconstituted
|
Dilution for test and Control (1/10 dilution)
|
Amount applied to container surfaceª
|
|---|---|---|---|---|
|
Cyclophosphamide
|
Sodium chloride 0.9%
|
20 mg/mL
|
2.0 mg/mL
|
0.0500 mg
|
|
Methotrexate
|
Sodium chloride 0.9%
|
25 mg/mL
|
2.5 mg/mL
|
0.0625 mg
|
|
5-Fluorouracil
|
Sterile Water for Injection
|
50 mg/mL
|
5.0 mg/mL
|
0.1250 mg
|
aProtocol: 0.025 mL in 4 droplets of approximately 6.25 microliters each, applied across a 7.6 cm by 10.2 cm (3-inch by 4-inch) area on the container surface.
RESULTS
TABLE 3 | Penetration of PAA/HP through Container Material of IV Bag over an 8-Hour (480 min.) Exposure Using a Procedure Based on ASTM Test Method F-7393
|
Container material
|
Average breakthrough detection time (minutes)
|
|---|---|
|
Polyvinyl chloride
|
>480
|
|
Propylene ethylene copolymer
|
>480
|
|
Polypropylene
|
>480
|
|
Ethylene vinyl acetate
|
>480
|
As shown in Table 3, the results of testing using ASTM F-739 on 4 types of polymeric films used in IV bags indicated no penetration or leaching (< 5 ppm) of PAA/HP solution through 8 hours of exposure in either study 1 (3 different areas, some may have contained seams) or study 2 (single samples that included bag seams).
The resistance of the IV bags to penetration from the PAA/HP solution was further substantiated by the results of testing using a commercially available assay for trace levels of hydrogen peroxide. As shown in Table 4, after soaking the 4 types of IV bags in the PAA/HP solution for 1 hour, the average concentrations of hydrogen peroxide recovered from the fluids inside the bags were below the minimum detection level of the method (<0.9 nanomoles/mL or 31 ppb). Although all the levels were below the minimum test threshold, the sodium chloride 0.9% from the 250 mL bags composed of PVC contained the highest concentration of peroxide of all the bag types. However, it was impossible to determine whether the increased levels were due to bag composition or to the smaller volume of the PVC bags.
Decontamination of 3 common hazardous drugs was accomplished by wiping the bags once with the PAA/ HP solution, waiting 3 minutes, then wiping the bags with sIPA (Figure 2). The average recovery efficiency of the HDs from the control bags (no wiping with PAA/HP) using the commercial HD sampling kit was approximately 78% (data not shown).
TABLE 4 | Concentration of Hydrogen Peroxide Measured in IV Bag Diluents after 1 Hour of Immersion in PPA/HP Solution using a Colorimetric Assaya
|
Container material
|
Container Volume
|
Mean Concentration of Hydrogen Peroxide†
|
Standard deviation
|
|---|---|---|---|
|
Polyvinyl chloride
|
250 mL
|
26
|
(13)
|
|
Propylene ethylene copolymer
|
1,000 mL
|
20
|
(15)
|
|
Polypropylene
|
1,000 mL
|
10
|
(5)
|
|
Ethylene vinyl acetate
|
500 mL
|
9
|
(1)
|
aThe minimum detection level of the method is <31 ppb.
†Measured in parts-per-billion (ppb)
With the test IV bags, a single pass of PAA/HP on quarter-folded wipes, followed by wiping with sIPA, reduced the average level of drugs by at least 99.97%. With all but 1 replicate with cyclophosphamide, no residual HDs (<10 ng per 7.6 cm x 10.2 cm area (3 inches by 4 inches) were detected after the decontamination protocol. The minimum detection level in these tests was 0.13 ng/cm2.
